If you or your near and dear one is suffering from esophageal cancer, you must be worried about the effectiveness of treatment options, side effects of the treatment, and managing symptoms such as difficulty swallowing or pain.
Esophageal cancer can be treated by esophagectomy which is a surgical procedure that, as per experts, can improve survival in patients by removing the tumor and affected tissues.
Esophagectomy is typically performed as part of a multidisciplinary treatment plan that may include other interventions such as chemotherapy, radiation therapy, or targeted therapies. The effectiveness of this procedure in improving survival depends on various factors, including the stage of the cancer, the presence of lymph node involvement, and the overall health of the patient.
One study suggests that en bloc esophagectomy may improve survival for patients with stage III esophageal cancer. En bloc esophagectomy involves removing the tumor and adjacent lymph nodes as a single unit.
Another study noted that adherence to quality measures during esophageal cancer treatment, including esophagectomy, is associated with improved survival.
What is esophagectomy?
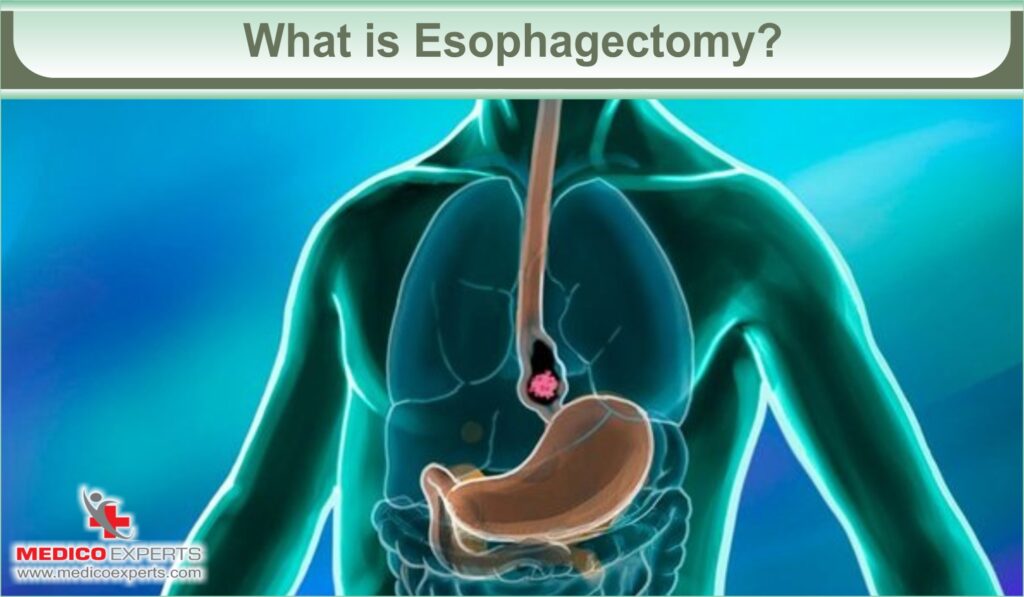
Esophagectomy is a surgical procedure to remove all or part of the esophagus, the tube that connects the throat to the stomach. It is performed to treat conditions such as esophageal cancer, severe acid reflux, or other diseases that affect the esophagus.
The exact steps of an esophagectomy can vary depending on the specific technique used and the surgeon’s preference.
Let us know about the steps involved in the esophagectomy surgery.
Step-by-Step Esophagectomy Procedure
- Preparation: The patient is prepared for surgery, which may include fasting, stopping certain medications, and receiving anesthesia.
- Incisions: The surgeon makes one or more incisions in the abdomen, chest, or neck, depending on the surgical approach. Different approaches include open surgery, minimally invasive (laparoscopic or robotic) surgery, or a combination of both.
- Mobilization: The surgeon carefully separates the esophagus, stomach, and surrounding tissues from other structures to ensure they can be safely removed.
- Lymph node removal: Lymph nodes near the esophagus may be removed to check for the spread of cancer.
- Esophageal resection: The surgeon removes the diseased part of the esophagus, leaving healthy tissue behind. The remaining esophagus is then reconnected to the stomach or another part of the digestive system.
- Reconstruction: In some cases, a portion of the stomach or another organ may be used to create a new conduit to replace the removed esophagus. This new conduit allows food and liquids to pass from the mouth to the stomach.
- Closure: The surgeon closes the incisions using sutures or staples.
- Recovery: After the surgery, the patient is closely monitored in the hospital. They may require a temporary feeding tube to provide nutrition while the newly reconstructed esophagus heals.
Minimally invasive esophagectomy (MIE)
There are several minimally invasive approaches to esophagectomy. Some commonly known types include:
- Minimally Invasive Transhiatal Esophagectomy: This approach involves accessing and removing the esophagus through small incisions made in the neck and abdomen.
- Minimally Invasive Ivor Lewis Esophagectomy: This technique combines laparoscopic and thoracoscopic approaches. The surgery involves removing the affected portion of the esophagus and reattaching the remaining part to the stomach.
- Minimally Invasive Three-Incision Esophagectomy: This approach utilizes three small incisions made in the chest, abdomen, and neck. It allows for the removal of the diseased esophagus and reconstruction with the stomach or other organs.
Complications of Esophagectomy Procedure
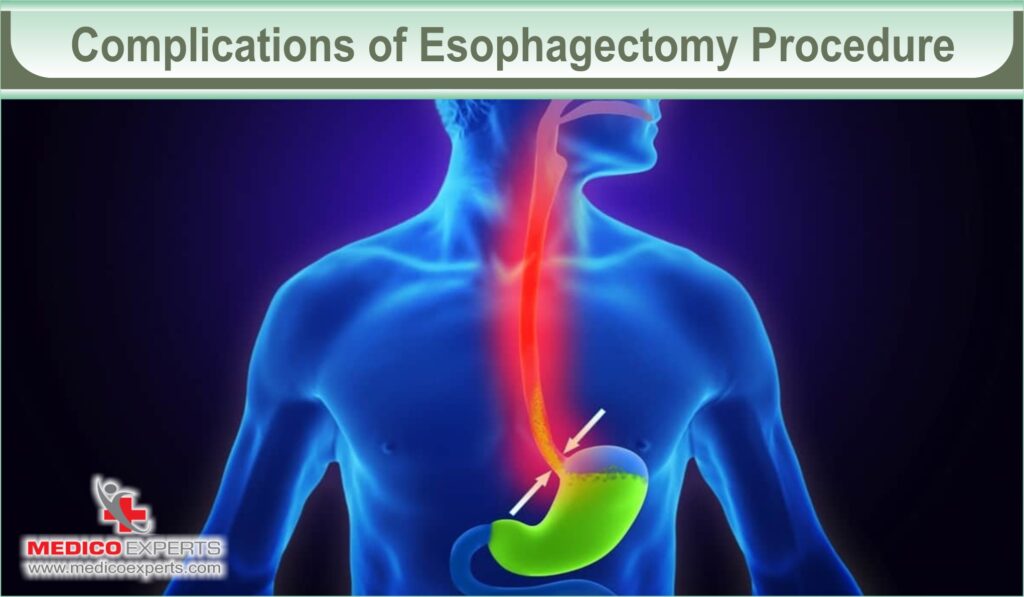
Esophagectomy is a complex surgical procedure, and like any surgery, it carries the risk of complications. Here are some common complications that can occur after an esophagectomy:
- Anastomotic leak: This is the most serious complication and occurs when the surgical connection between the remaining esophagus and the stomach or other parts of the digestive tract develops a leak. It can lead to infection, abscess formation, and other complications.
- Bleeding: Surgical bleeding can occur during or after the procedure and may require further intervention to control.
- Infection: Infections can occur at the incision sites or in the chest or abdominal cavities. They can be treated with antibiotics, but in severe cases, additional surgical procedures may be needed.
- Pneumonia: Some patients may develop pneumonia after the surgery due to impaired lung function and the risk of aspiration.
- Delayed gastric emptying: After an esophagectomy, the stomach may take longer to empty, leading to symptoms such as bloating, nausea, and vomiting.
- Reflux: Reflux of stomach acid or bile into the esophagus can occur after the surgical procedure, causing heartburn and other symptoms.
- Dumping syndrome: This condition can occur when food moves too quickly from the stomach into the small intestine, causing symptoms such as diarrhea, nausea, and lightheadedness.
- Chylothorax: This is a rare but potentially serious complication that occurs when lymphatic fluid leaks into the space around the lungs, leading to difficulty breathing.
- Voice changes: Surgery near the vocal cords can sometimes lead to changes in voice quality or hoarseness.
- Cardiac complications: Patients with pre-existing heart conditions may be at risk for complications such as arrhythmias or heart attacks.
What is the Success Rate of the Esophagectomy Surgery?
The success of an esophagectomy procedure can be measured in various ways, including the rate of complications, and the long-term survival rate.
Complications:
Esophagectomy is a complex surgical procedure that carries a risk of complications. Some common complications include hemorrhage, infection, leakage of digestive fluids, narrowing of the remaining esophagus (strictures), and respiratory problems.
The incidence of complications can vary depending on the type of surgery (open surgery vs. minimally invasive surgery) and the experience of the surgical team. However, advances in surgical techniques and perioperative care have helped reduce the incidence of complications.
Survival rate:
The long-term survival rate after esophagectomy depends on several factors, including the stage of the esophageal cancer at the time of surgery. According to a study published in Pubmed, the 5-year survival rate for esophageal cancer is around 15% to 25%.
However, it is worth noting that survival rates have improved over the years due to advancements in surgical techniques.
What is the cost of the Esophagectomy Procedure?
The cost of Esophagectomy in India is $4,500 (INR 330,500) and is the main reason for attracting medical tourists in India.
Conclusion
Esophagectomy is a surgical procedure performed to remove all or part of the esophagus, usually due to esophageal cancer. The procedure can be performed using different approaches, such as minimally invasive techniques.
Complications can occur after esophagectomy, including hemorrhage, infection, leakage, strictures, and respiratory problems. However, advancements in surgical techniques and perioperative care have helped reduce the incidence of complications.
Esophagectomy can have an impact on a patient’s quality of life, particularly in terms of swallowing function and nutrition. Postoperative care and rehabilitation are important for improving quality of life.
MedicoExperts has an expert panel of doctors and surgeons who not only take care of the surgery but also pay attention to the quality of care post-operation and follow-up.
FAQ :
Q1. What is the life expectancy after an esophagectomy?
The median time of survival after transthoracic or transhiatal esophagectomy was 20.5 months and 16.4 months, respectively.
Q2. Can you eat again after esophagectomy?
You will be on a liquid diet just after surgery. Then, you are advised to take soft foods till 8 weeks from surgery.
References
https://pubmed.ncbi.nlm.nih.gov/9434690/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7656435/
https://www.frontiersin.org/articles/10.3389/fsurg.2022.893429/full



